There Will Always Be a Need for Physicians and Surgeon and Becoming One is an Easy Process
Sign up for Derek's newsletter here.
By the time Elizabeth Erickson was a freshman at Davidson College in 2002, she knew she wanted to become a doctor. Because she understood that the earliest health interventions are among the most important, she set herself on a pediatrics track. After four years of premed classes, she went straight to medical school at Wake Forest University, which took another four years. Then came three years of residency at Duke University, plus one final year as chief resident. In 2014, she joined the faculty of Duke's School of Medicine. Her dream was realized at the steep price of 12 consecutive years of learning and training, plus about $400,000 of debt.
Erickson's story would be exceptional in just about any other country. But it's hardly unusual in the United States, which has the longest, most expensive medical-education system in the developed world, and among the lowest number of physicians per capita. "There is a huge scarcity of primary-care doctors, like pediatricians, and many of us are operating in a scarcity framework without enough resources," Erickson told me.
In January, I wrote that America needs an abundance agenda—a plan to attack the problems of scarcity in our housing, infrastructure, labor force, and, yes, health-care system. As the pandemic has made clear, we need medical abundance in the 21st century. That means more high-quality therapies, more clinics, better insurance, and better access to medicine. But it also means more doctors.
As I dug deeper into the roots of America's health-care scarcity, I realized that I had to start by answering a simple question: Why does America make it so hard for people like Elizabeth Erickson to practice medicine?
Imagine you were planning a conspiracy to limit the number of doctors in America. Certainly, you'd make sure to have a costly, lengthy credentialing system. You would also tell politicians that America has too many doctors already. That way, you could purposefully constrain the number of medical-school students. You might freeze or slash funding for residencies and medical scholarships. You'd fight proposals to allow nurses to do the work of physicians. And because none of this would stop foreign-trained doctors from slipping into the country and committing the crime of helping sick people get better, you'd throw in some rules that made it onerous for immigrant doctors, especially from neighboring countries Mexico and Canada, to do their job.
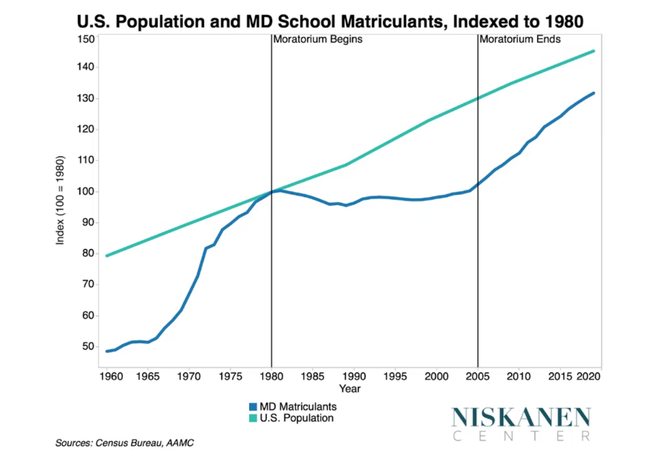
Okay, I think you've caught on by this point. America has already done all of this. Starting in the late 20th century, medical groups asserted that America had an oversupply of physicians. In response, medical schools restricted class sizes. From 1980 to 2005, the U.S. added 60 million people, but the number of medical-school matriculants basically flatlined. Seventeen years later, we are still digging out from under that moratorium.
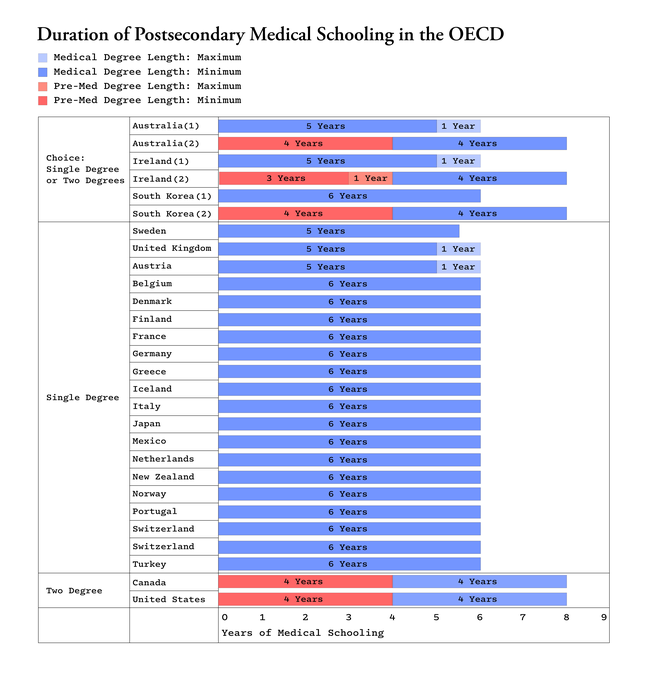
The U.S. is one of the only developed countries to force aspiring doctors to earn a four-year bachelor's degree and then go to medical school for another four years. (Most European countries have one continuous six-year program.) Then come the years of residency training. Many graduates have $200,000 to $400,000 in outstanding student loans when they enter the workforce. Medical education is a necessary good; nobody wants charlatans in the OR and snake-oil salesmen prescribing arthritis medication. What I'm asking is: What advantage do these additional years and loans get us? I suppose it's conceivable that American doctors are 33 percent better than Swiss doctors, given our 33-percent-longer medical schooling. But good luck trying to find a national health statistic where the U.S. is one-third better than Switzerland. Americans die earlier than their European counterparts at every age and income level.
Overburdened with debt and eager to translate their long education into a high salary, American medical students are more likely to become specialists, where they tend to earn some of the highest doctor salaries in the world, in part because the U.S. does such an efficient job at limiting the supply of their labor.
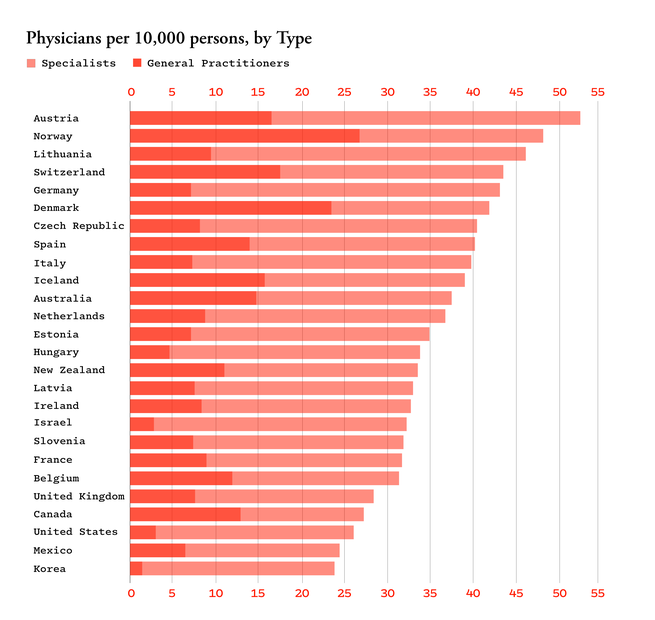
As a matter of basic economics, fewer doctors means less care and more expensive services. A 2016 survey of patients in 11 countries—the U.S., Canada, New Zealand, and eight European nations—found that the U.S. trailed in providing timely access to primary medical care. High educational debts and fewer physicians push more health-care spending toward intensive and specialized services, which are more costly.
Naturally, some doctors might object to more competition for the same reason that some homeowners object to more local construction: They're afraid that abundance will eat their wealth. But they should consider the other side of the coin, which is that having more doctors might make life better for doctors, who work much longer hours than their European peers. Doctor burnout and brutal 16-hour shifts for residents and M.D.s aren't necessary tests of willpower; they're just the inevitable result of not having enough people to do the work that today's hospitals demand.
The most obvious reason America needs an abundance of medical practitioners is … just look around. If COVID continues to be a problem for the U.S.—and that seems likely—we're going to need more physicians, clinics, and therapies. Even if COVID disappears and the U.S. never faces another pandemic ever again (he wrote, fingers and toes crossed, after throwing a whole thing of salt over his shoulder), we'll be an older and aging country with more sick people. The census projects that in 12 years, there will be more senior citizens than children in America for the first time in history. No matter what the pandemic future holds, we need more doctors to be part of America's health-care system.
So how do we solve the problem? That's the question I posed to Robert Orr, a policy analyst who studies health-care policy at the Niskanen Center.
"The first thing I would do is to expand the residency system so that more doctors can become residents after medical school," Orr told me. "This might be the key bottleneck. The medical schools say they can't easily expand, because there aren't enough residency slots for their graduates to fill. But there aren't enough residency slots because Washington has purposefully limited federal residency financing." The arithmetic is simple: More funding means more residents; more residents allows medical schools to grow; more medical students today means more doctors in a decade.
Countries get doctors in one of two ways—by training them or importing them. We're bad at both. When NAFTA was negotiated, Canadians and Mexicans didn't want to lose their doctors to the American market, and the U.S. didn't want immigrant doctors to threaten U.S. physicians. As a result, to this day Mexican and Canadian doctors have to jump through special hoops to practice medicine full-time in the U.S.
Beyond increasing the number of doctors, states could increase the total supply of care by allowing more nurse practitioners to substitute for doctors. They could also expand legal telemedicine, which would extend care to rural and other underserved areas. "The low-hanging fruit is to change Medicare rules so that the government would reimburse for all online appointments," Orr said. This would drive the permanent adoption of telemedicine throughout the system.
Finally, Orr said that we can't expand the number of doctors unless we also expand the number of clinics and hospitals, particularly in the most underserved parts of the country. That means we have to build. "We need a system of health-care-development banks that issue guaranteed loans for infrastructure projects," he said. "That's how the health-care system was originally built up until the 1980s, with government-backed finance."
More doctors, more clinics, more care, better health outcomes. It all sounded so obvious—too obvious. So, at the end of our conversation, I asked Orr to imagine all the ways we might be wrong. What's the problem with an abundance of doctors?
We thought of several downsides. More physicians could mean lower wages for doctors. If wages dropped before student debt declined, that would mean a generation of doctors graduating with hundreds of thousands of dollars of debt that they are unable to pay off in a more competitive market. Orr said that expanding the role for the nurses we have might be politically easier than radically changing medical education to grow the number of doctors, and that tweaking immigrant-doctor rules could raise the ire of physician groups. "Another steelman to my case that you might hear is that America should focus on prioritizing high-value care rather than just aimlessly expanding medical providers who do a lot of low-value stuff," he said.
But overall, the case for doctor abundance is strong. Sick, aging, and buckling under two years of pandemic mayhem, America desperately needs more physicians. But we choose to make becoming a physician a painful experience. Today we are reaping the harvest of our deliberate policies: fewer doctors, higher prices, and worse access to primary care.
Source: https://www.theatlantic.com/ideas/archive/2022/02/why-does-the-us-make-it-so-hard-to-be-a-doctor/622065/
Post a Comment for "There Will Always Be a Need for Physicians and Surgeon and Becoming One is an Easy Process"